HEALTH PROGRAM MATERNAL AND CHILDREN
The health program Mother and Child's mandate is to promote a healthy pregnancy and a healthy baby. by accompanying pregnant women throughout their gestation period and by offering clinical follow-ups with the doctor and/or nurse. In addition, the program provides parents with education, support and appropriate referrals to other community services so that mothers and babies reach a standard. of health optimum. The program teaches and coaches new parents in their role and in their ability to to ensure the well-being and healthy development of their children.
Eligibility Criteria
Be a patient member of the CMSA and have a positive pregnancy test and/or have a small child between 0 and 6 years old in need of medical follow-up and vaccination.
Pregnant women with a complex pregnancy or risk of complications, according to the evaluation of the attending physician, will be referred to genecology for their pregnancy follow-up.
Prenatal care
- Important Information
- Pregnancy in trimesters:
- First trimester: 0 – 13 weeks
- Second Trimester: 14 – 28 weeks
- Third trimester: 29 – 40 weeks
- Frequency of antenatal visits:
- < 28 weeks: Every 4 – 6 weeks
- 28-36 weeks: Every 2-3 weeks
- > 36 weeks: À every week
- Prenatal care can be provided by:
- Family doctor
- Nurse Practitioner
- Obstetrician
- Midwife
- Pregnancy in trimesters:
- Screeningto measure health. of your pregnancy
- First trimester (usually done between 11 and 14 weeks):
- Urine test: Screening for pregnancy complications and urinary tract infections. Tests for the presence of sexually transmitted infections that can be treated with antibiotics for pregnancy.
- Blood test:
- PAPP-A and HSG: used to screen for complications related to pregnancy
- Anaemia (lack of healthy red blood cells)
- Blood type and rhesus factor: May signal incompatibility. potential between your blood type and that of your baby. You may need the injection of WinRho at the end of your life. 28 weeks and 72 hours postpartum
- Hepatitis B infection
- Immunity rubella: You will need an MMR vaccine after delivery if no immunity
- Ultrasound: To confirm your due date. Can be completed as early as 7 to 10 8 weeks gestation.
- Tests may be done to determine your baby's risk of has certain chromosomal conditions, especially Down syndrome (trisomy 21) and extra sequences of chromosome 18 (trisomy 18)
- Optimized first trimester screening (DPTO): This process will require a blood draw and your provider to perform a special ultrasound. This ultrasound measures the clarity of nuchal (the size of the free space in the tissues at the back of your baby’s neck), which can help in the diagnosis of chromosomal abnormalities.
- Non-Invasive Prenatal Testing (NIPT): A blood test that analyzes DNA fragments circulating in maternal blood and screens for chromosomal conditions. * This test may require payment if not covered by insurance.
- Additional test:
- Chorionic villi sampling (CVS): If the NIPT or ultrasound is abnormal, your healthcare provider may recommend a CVS. This is a diagnostic test that will take a small sample of the placenta, which contains your baby’s genes, and can confirm or rule out that your child has a chromosomal disorder. This is usually done between 10 and 13 weeks of pregnancy.
- Second trimester (usually done between 15 and 22 weeks) - The results of your first trimester screening may be combined with others that are performed ;s during the second trimester to give you a more accurate understanding of health. of your baby
- Urine test
- Blood test
- &Echography– to examine your baby’s anatomy, growth and behavior, to check the amount of amniotic fluid, to examine blood flow patterns and to measure the length of the cervix.
- Glucose Tolerance Test – for the presence of gestational diabetes, a type of diabetes that occurs during pregnancy and affects approximately 6 – 9% of all pregnant women. Usually performed between 24 and 28 weeks of gestation. For the test, you will drink a special sugary drink and then give a blood sample. A second test may be needed if your results are abnormal.
- Your baby's heartbeat are much clearer and more easily detectable during the second trimester. It would be a good time to listen to them!
- The gender of your baby can be determined around 18 weeks of pregnancy.
- Additional test
- Amniocentesis: This test may be offered to women at risk (e.g. 35 years or older) and is usually performed between 16 and 20 weeks of gestation. It can detect hundreds of genetic and chromosomal abnormalities. It involves inserting a long, thin needle into your abdomen and uterus to draw amniotic fluid which will then be sent to your uterus. to a lab for testing.
- Third Trimester (usually performed at 29 weeks, 36 weeks, and weekly thereafter) – During this trimester, routine biophysical profiles or reactivity exams fetal gas may be necessary for long-term pregnancies. high risk.
- Urine test
- Blood test
- Ultrasound: To monitor fetal growth, determine the position of the baby. and assess the placenta.
- Group B Strep Test: Group B Strep (GBS) is a type of bacteria found in the vagina and rectum. It is harmless to you, but it could cause an infection in your baby. when exposed to the bacteria during childbirth. The test is usually performed around 36 weeks and consists of swab your vagina and rectum during a pelvic exam. If it is positive, you will be treated with antibiotics during labour. About 25% of women are positive for GBS.
- Reactivity test Fetal Monitor (NST): During an NST, a fetal monitor will be placed around your belly to monitor your baby's heart rate. for about 20-40 minutes. Your healthcare provider may recommend follow-up testing with a biophysical profile if the NST is atypical.
- Biophysical Profile (BPP): To determine if labor should be induced. The test uses an ultrasound to measure your amniotic fluid levels and assess heart rate, movement, tone (i.e. the ability to flex a limb) and pain. your baby's breathing. If the results are abnormal, your healthcare provider may recommend an early delivery.
- Pelvic exam: Usually done towards the end of your pregnancy and is used to determine if the cervix has started the process of maturing for birth.
- First trimester (usually done between 11 and 14 weeks):
Postnatal care
1. Important information:
To prepare for your appointment
- Bring a list of your questions and concerns so you don't forget anything;
- Consider bringing your partner (or other primary caregiver). Two people can more effectively care for your baby, remember provider advice, and remember questions to ask. pose.
What to bring for your baby
- To the first appointment after the birth, bring the documents from the hospital containing information about your baby’s weight. to discharge and complications of your pregnancy and/or childbirth;
- Dress your baby; with simple clothes and bring a blanket;
- Bring a change of clothes, extra diapers, wipes, pacifiers, feeding supplies, and other necessities.
Postpartum and baby care healthy can be delivered by a:
- Family doctor
- Nurse Practitioner
- Obstetrician
- Midwife
- Pediatrician
2. Health Checkup postpartum for mom:
Usually programmed; Between 3 and 6 weeks after giving birth, a postpartum checkup is an appointment after birth with your care provider to check how you are doing physically, mentally, and emotionally after giving birth. had a baby. This is usually one or two meetings, but you may need more depending on your specific situation and circumstances. Here's what to do what you can expect on appointments:
- Breast examination;
- Pelvic exam and possibly Pap smear;
- Checking weight and blood pressure;
- &Evaluation of diet to determine if you need supplements like calcium and iron;
- Follow-up for pregnancy complications (e.g. blood sugar test if you had gestational diabetes);
- Physical examination to assess if your uterus is shrinking her pre-pregnancy size, make sure any incisions (e.g. episiotomy or caesarean section) heal properly and discuss common postpartum symptoms such as bladder problems, bleeding and postpartum cramps, hemorrhoids, etc.;
- Discussions about resuming activities such as:
- Physical exercises
- Sexual relations
- Contraception
- Discussions about your health mental health and your plans for subsequent pregnancies, if any.
3. Health Checkup for baby and child:
The visits of the baby; healthy or “ Well-Baby» are a time when you can meet with your healthcare provider and have your health checked. of the baby to make sure he is growing and developing normally.
*Babies should have their first health visit in the week following their leave from the hospital and their return to home.*
Thereafter, follow-up appointments should take place at: 1 month, 2 months, 4 months, 6 months, 9 months, 12 months, 15 months, 18 months and 24 months. (This is the recommended schedule, but the baby's caregiver can change it.)
During a baby visit healthy , you will first fill out electronic questionnaires when you come to the office. the reception. Then your baby will be seen by a nurse who will:
- Weighing your baby ;
- Measure height and head circumference;
- Asking introductory questions about yourself and health of your child;
- Administer required vaccinations (see Ontario's vaccination schedule below).
Then your care provider will:
- Perform a head-to-toe assessment;
- Ask you about their eating habits;
- Ask you about their sleeping habits;
- Ask yourself about your baby's developmental milestones
- Provide necessary counseling (e.g. safe sleep practices, eating issues, health issues, etc.)
- Being available to answer your questions; all your questions and concerns.
Finally, the nurse will administer the vaccines to the patient. the end of the visit to avoid distress during the appointment.
See the following website for the latest version of Ontario's publicly funded immunization schedule: https://www.health.gov.on.ca/en/pro/programs/immunization/docs/Publicly_Funded_ImmunizationSchedule.pdf below
Following postpartum and baby check-ups In health, your care providers may refer you to other internal programs such as the nutrition program or the Prisme program for psychosocial services depending on your needs. For more details on these programs, please refer to the sections at: this effect elsewhere on this website.
Corridor of referrals to external partners
- Laboratory for prenatal blood screening
- Ultrasound of date and development
- Prenatal Screening Ontario
- Obstetrician
- Midwife
- Pediatrician
- Newborn Care: Monarch Center Center
- Health City of Ottawa public services and resources: ‘Parenting Ottawa’
- https://www.parentingaottawa.ca/en/shared-content/ourservices.aspx
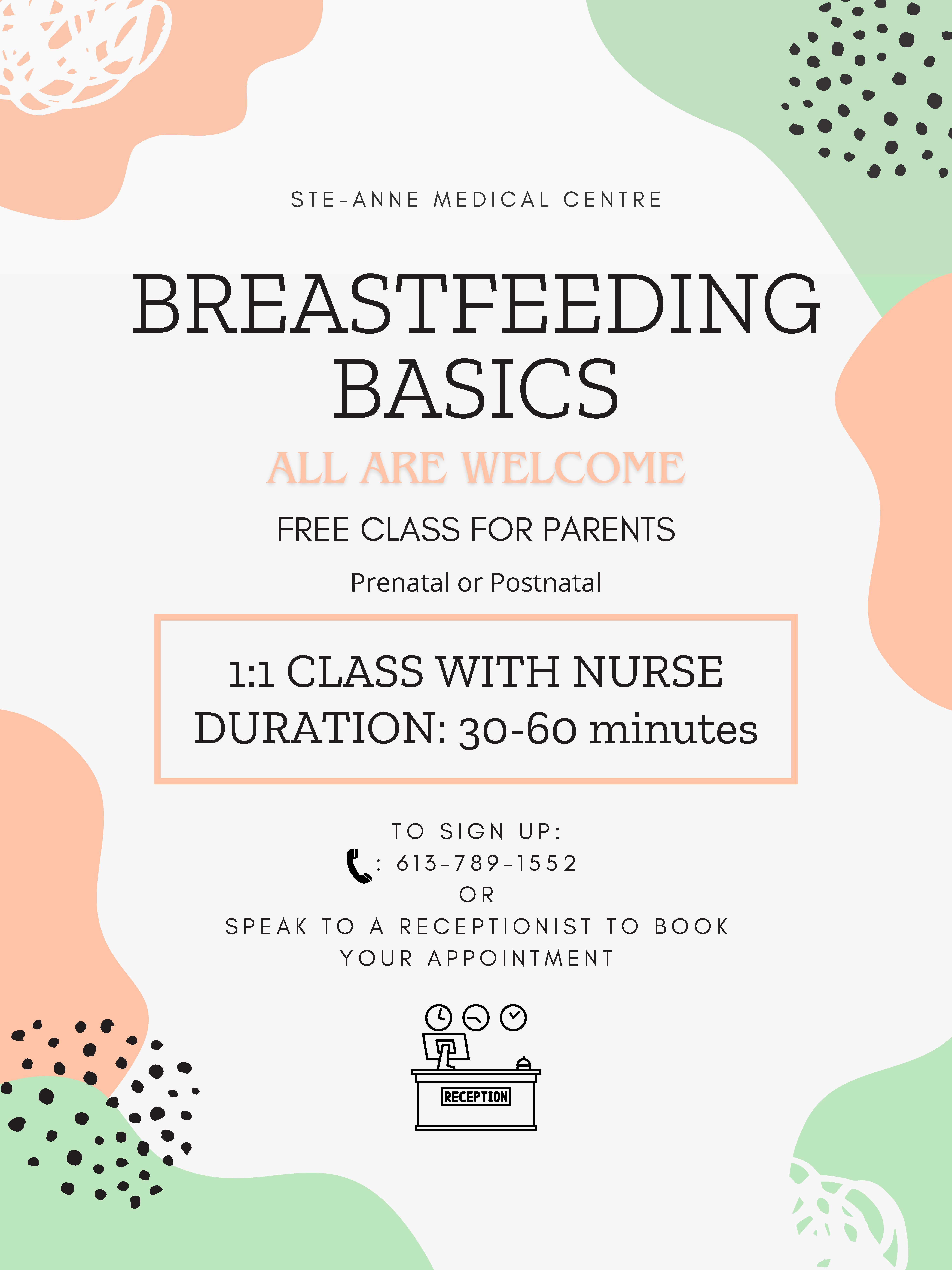
- prenatal classes
- online support
- telephone support
- peer parenting support
- visits to; home
- crossroads
- support for; breastfeeding
- https://www.parentingaottawa.ca/en/shared-content/ourservices.aspx
- Éparental educationChamplain LHIN: ‘ Çsimmered’
- Educational Centers
- Community resource center in your neighborhood